Ref: Charing Cross Vascular Symposium 2015 + EndovascularToday
Atherosclerotic lesions affecting runoffs in diabetic patients are super challenging: crossing the lesion, debulking the calcified atheroma, and avoiding arterial dissection for the, commonly, only runoff artery are some of the many challenges that faces the treatment process.
Few tips and tricks have emerged over the years that can provide a good framework to approach those lesions, and avoid major limb amputation if possible.
Crossing the lesions-
- This article describes some useful tips for crossing those lesions: http://evtoday.com/pdfs/et0513_FT_csi.pdf
- Dilate the distal microvasculature with an infusion of 200 to 400 μg of nitroglycerin, administered through the sheath before initial treatment. Additional nitroglycerin boluses of up to 400 μg are suggested after every second treatment.
- Administer systemic anticoagulation with intravenous heparin (100 IU/kg).
- Possibly run heparin saline infusion through the supporting catheter to provide a jet stream with the GTN.
- Can we consider using a vasodilator other than GTN? Currently, Iloprost is not licensed in the UK (even to be given intravenously). It should then be only allowed on an off-license basis under a specialist advice exclusively. Patient should be well informed. This is then accepted to be delivered as an IV (despite some RCTs delivering this from within the bypass graft). The efficiency of Iloprost is to be determined. There is currently no clear evidence that Iloprost will dilate the vasculature bed and help the cannulation process whatsoever. GTN is probably much better to use. Papaverine is also well known for its effect (unlicensed).
- If doing popliteal/TPT endarterectomy before crossing the distal lesion, then ensure avoiding to reach the small arterial lumen with your dissection. Once reached, it would be so hard to keep the lumen open without a dissection flap, which can fully compromise the lumen access later on. You can complete your endarterectomy once an access to the true lumen is well established, and the perfusion started.
- Cross the lesion with the 0.014-inch ViperWire Advance® guidewire and position the guidewire tip to make sure there is sufficient distance between the guidewire spring tip and the distal end of the shaft (10-cm minimum at all times). The ViperWire Advance® should be within the true lumen of the vessel; subintimal use of the device may be ineffective.
- If the ViperWire Advance® cannot be placed as a primary guidewire, use a stepwise approach to cross the lesion with a specialized crossing guidewire. A support catheter, such as Quick-Cross (Spectranetics Corporation, Colorado Springs, CO), may facilitate guidewire placement.
Angioplasty +/- Drug Coated Balloons +/- Drug Eluting Stents – what is the evidence so far?
- The following few points explains the current understanding in performing distal endovascular procedures (Charing Cross Vascular Symposium 2015), delivered by Prof Thomas Zeller:
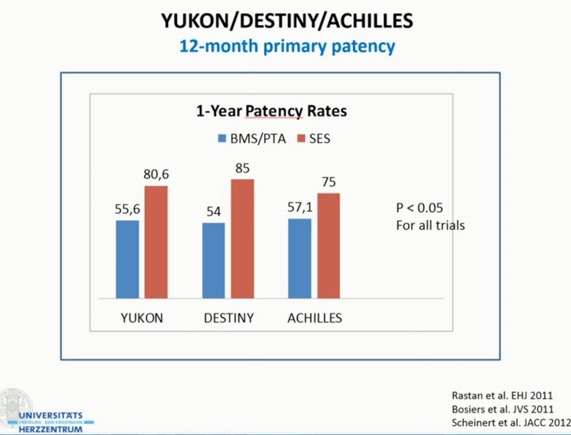
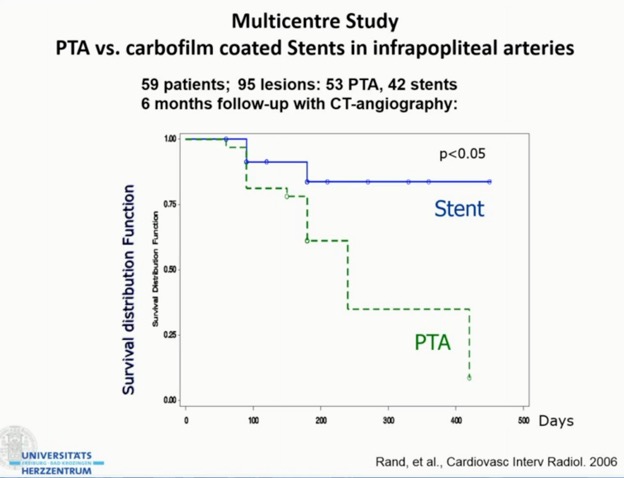
- Use drug eluting stents (DES) in lesions < 10 cm ?PRIMARILY. Current trials support the superiority of Self-expanding (Nitinol) stents (SES) over PTA or Bare-Metal Stents only, for 12-24months follow up.
- For lesions >10cm, use drug coated balloons (DCB) primarily. RCTs (IN.PACT, DEBATE) supports their use over PTA or DES.
- Atherectomy – this is indicated in diffuse fibrotic and calcified lesions, and in preparation for DCBs.
-
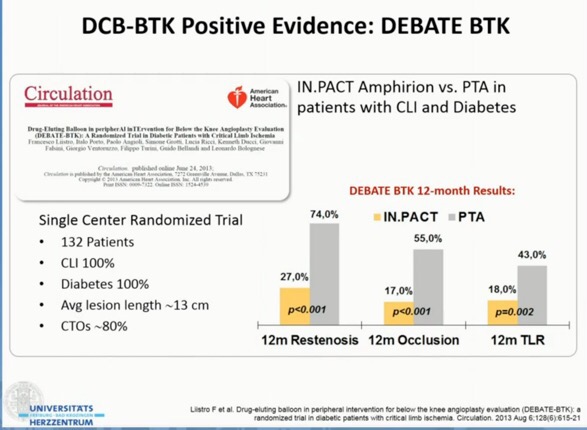
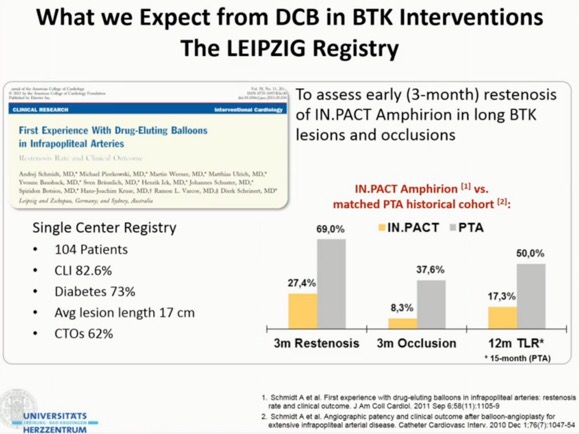
- The following presentation summarises the current understanding/evidence behind this area.