Which is better long-term: endovenous laser ablation or traditional surgery for varicose veins?
Ref: EJVES Nov 2015
This is seriously interesting!! Most, if not all, surgeons have now ‘switched to’ endovenous thermal ablation (laser or RF). The endovenous therapy has proven safety and mid-term results. what about the long term recurrence? RELACS study has some logic : traditional surgery risks the recurrence to occur in the site of operation; the endothermic risks the recurrence to occur in other places. Here are the results:
Same Site Recurrence is More Frequent After Endovenous Laser Ablation Compared with High Ligation and Stripping of the Great Saphenous Vein: 5 year Results of a Randomized Clinical Trial (RELACS Study)
Interventions were performed on ambulatory and hospitalized patients at two vein centres, a university dermatology department (EVLA) and a specialized vein clinic (HLS). Four hundred patients suffering from GSV incompetence were assigned to EVLA or HLS of the GSV. One hundred and eighty five and 161 patients (=limbs), respectively, were treated per protocol. Main outcome measures were clinically recurrent varicose veins after surgery (REVAS classification, primary study objective), Duplex detected saphenofemoral recurrence, clinical venous severity scoring (Homburg Varicose Vein Severity Score), quality of life (Chronic Venous Insufficiency Questionnaire 2), side effects, and patient satisfaction 5 years after treatment.
Results
- Two hundred and eighty one legs (81% of the study population) were evaluated with a median follow up of 60.4 (EVLA) and 60.7 months (HLS).
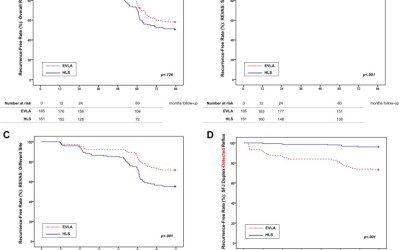
- Overall, REVAS was similarly observed in both groups: 45% (EVLA) and 54% (HLS), p = .152.
- Patients of the EVLA group showed significantly more clinical recurrences in the operated region (REVAS: same site): 18% vs. 5%, p = .002.
- In contrast, more different site recurrences were observed in the HLS group: 50% vs. 31%, p = .002.
- Duplex detected saphenofemoral refluxes occurred more frequently after EVLA: 28% vs. 5%, p < .001.
- Both treatments improved disease severity and quality of life without any difference.
The results are summarised in this good figure:
The figure is shown for educational purposes only and not for reuse.
Conclusion – don’t take it for granted!! need more work on best treatment options …
CERAB technique to replace aorto-bifemoral bypass .. is heating up!
Ref: EJVES Nov 2015
This is the editor’s choice for EJVES this month… and it deserves!! It is a new era in major vascular reconstruction, now been followed for 0-48 months with excellent results so far. The study took place in the Netherlands and in Belgium.
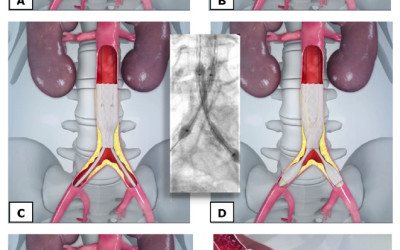
The procedure is simply to use covered stents after passing the iliac and aortic blockage with wires and catheters.
picture taken from CERAB original description for educational purposes only. http://www.angiocare.nl/uploads/downloads/4.CERAB_ZNA_poster-(1).pdf
The idea resembles the EVAR technique, with three key differences: passing wires through blockages; landing in a less-than-average aortic diameter, and lack of further attachments (barbs, hooks, etc.).
Between 2009 and March 2014, 103 patients (51 male, 52 female) suffering from obstructive lesions at the level of the aortic bifurcation were treated with CERAB in two clinics. The median age was 61 years (range 36–85 years). Lesion morphology was evaluated by CT angiography. Six TASC-II B lesions, nine TASC-II C lesions, and 88 TASC-II D lesions were treated. Follow up was a median 12 months (range 0–49 months) and consisted of clinical examination, ankle brachial indices, and duplex ultrasound examination.
- Technical success was obtained in 98 procedures (95.1%). In five cases lesions could not be recanalized.
- Primary patency was 87.3% at 1 year and 82.3% at 2 years, while secondary patency was 95.0% at 1 year and 95.0% at 2 years.
- Mean ankle brachial indices improved significantly from 0.64 ± 0.21 before to 0.91 ± 014, after the procedure (p < .001).
- The overall 30 day complication rate was 23.3%, including 22 minor complications and two major complications (1.9%).
- There was no 30 day mortality. Median hospital stay was 2 days (range 1–16 days).
What this paper adds
The study is an evaluation of the first (and largest) patient cohort, showing the safety and excellent patency of this technique when treating aortoiliac arterial occlusive disease. There seem to be a potential shift from open surgical bypass grafting to endovascular treatment for patients suffering from disabling intermittent claudication or critical limb schema. We need more info and longer term results to judge; but the astonishing 0% mortality and 2 day LOS is impressive so far, not to mention the 95% technical success rate.