I have put the following tool to easily calculate the risk of performing AAA surgery, based on GAS, VBHOM, and vPOSSUM. I have also added a new self-designed interesting monogram, a rupture index tool, that I found fascinating in calculating the risk of rupture in patients with AAA.
Treatment of varicose veins – time for CCG to change their attitude
ref. NICE Guidelines Aug 2014 – Link
NICE has made it clear that it is time to change the attitude and offer endothermic/foam/and even surgery for patients who are likely to be struggling with their varicose veins permanently BEFORE going into the compression hosiery option.
This is what they stated, and this is what I used recently in a letter to the GP requesting for funding (the outcome of which is not known yet!):
“Historically surgery and compression therapy were the only treatments available to people with varicose veins, but in recent years other treatments including endothermal ablation and ultrasound-guided foam sclerotherapy have been developed. These newer therapies are less invasive than surgery, promote faster recovery and need shorter hospital stays.
NICE has made it clear that it is time to change the attitude and offer endothermic/foam/and even surgery for patients who are likely to be struggling with their varicose veins permanently BEFORE going into the compression hosiery option.
This is what they stated, and this is what I used recently in a letter to the GP requesting for funding (the outcome of which is not known yet!):
“Historically surgery and compression therapy were the only treatments available to people with varicose veins, but in recent years other treatments including endothermal ablation and ultrasound-guided foam sclerotherapy have been developed. These newer therapies are less invasive than surgery, promote faster recovery and need shorter hospital stays.
People with varicose veins are offered treatment with:
- endothermal ablation (in which the veins are closed off using heat)
- or, if endothermal ablation is unsuitable, a treatment called ultrasound-guided foam sclerotherapy (in which the veins are closed off using a chemical foam)
- or, if both endothermal ablation and ultrasound-guided foam sclerotherapy are unsuitable, surgery to remove the varicose veins.
They should only be offered compression hosiery (stockings designed to improve blood flow by squeezing the legs) as a permanent treatment if none of the other treatments are suitable for them.
Vascular bed-side teaching curriculum – a DGH experience
It’s important, and interesting, to lead on the quality and quantity of core vascular knowledge that you deliver to trainees (FY1/2, CT1-3, STs) during your ward rounds … regardless of how many ward rounds you do (once weekly; once every six weeks, etc.).
The following topics and depth of vascular knowledge have to be delivered during your ward rounds; its up to you to design how and over what time you are delivering them.
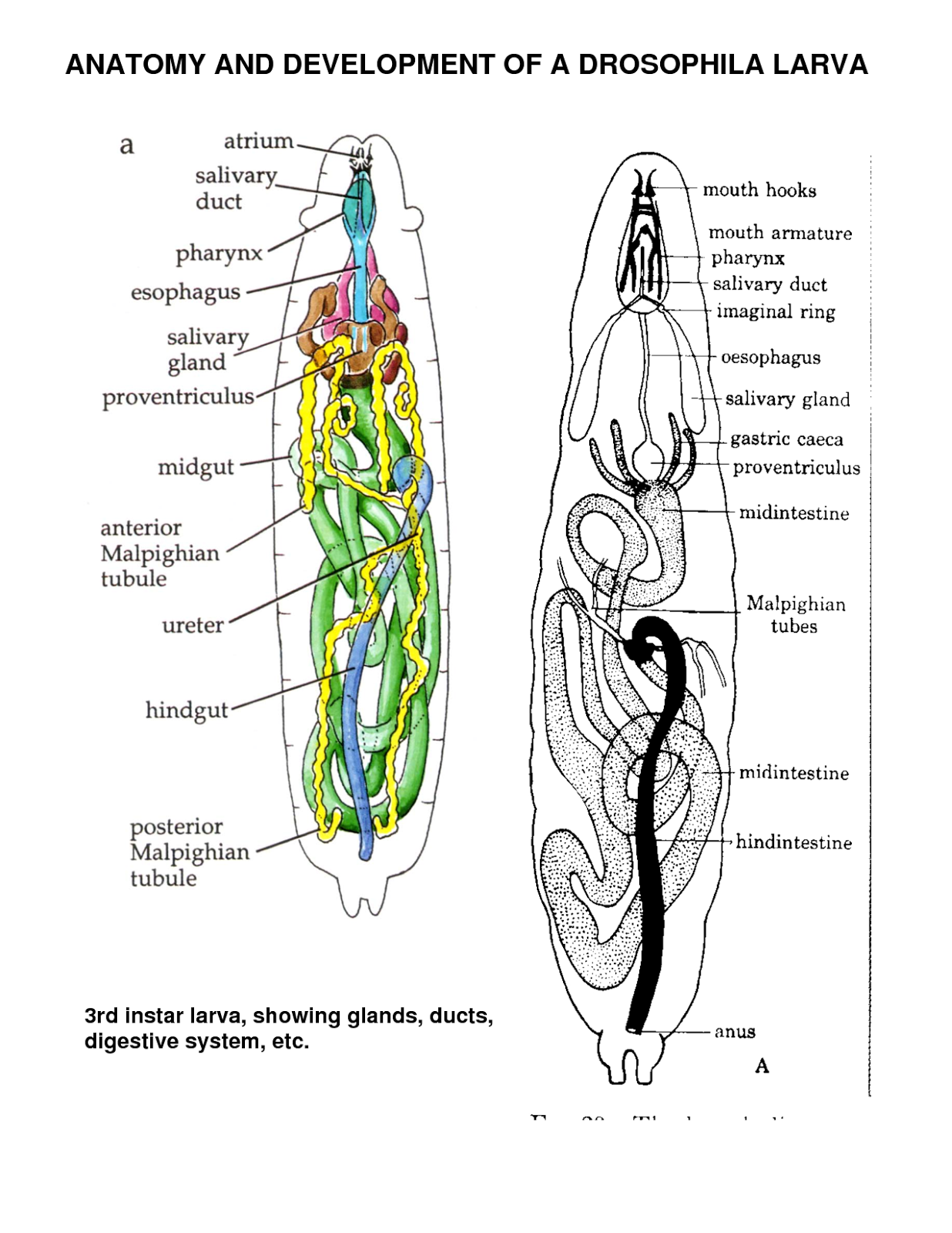
- Basic vascular anatomy and surface anatomy: the tree; origin; branches; access and important structures; essential landmarks
- Basic history and physical examination of the six types of vascular diseases: ICs (with emphasise on risk factors and exercises/smoking); CIL (with emphasis on definitions and correlation to pressures); AAA (with emphasis on acute presentation and decision making); VVs (with emphasis on classification and severity); and diabetic foot (with emphasis on changes in skin, muscles, bones, deformities, nerves, and circulations).
- Core vascular ultrasound scan / waves/ resistance/ eABPIs/ pitfalls/
- Core pathophysiology – atherosclerosis (stages; endothelium; effect of statin; combination of organ effect) – aneurysmal disease – varicose veins – CILs – diabetic foot – see MRCS presentation
- Core principles of biomechanics in diabetic foot. – see biomechanics presentation
- Vascular Facts and Figures
- Basic techniques in vascular surgery:
- CORE VIDEOS
- EXPOSURE: aorta; iliac; femoral; popliteal; foot; carotid; subclavian; axillary; brachial;
- PROCEDURES –
- LEVEL OF COMPETENCY I would expect from a vascular trainee (with different levels of course):
PROCEDURES TO BE DISCUSSED (TO DIFFERENT LEVELS):
Venous eczema
This is the best solution I have ever found when a venous eczema is not responding to radiofrequency treatment; or when a skin graft is not taking:
The DFZ regime
Fucibet 30g x4tubes daily for 2/52
Zip Zoc bandage x14 apply daily
Dermal lotion 500 apply regularly to skin
Excellent results indeed!!
Interesting vascular history
Wiliam and John Hunter …
Scottish brothers … born in 1718 and 1728; William was a dedicated educated person .. John never enjoyed books but was fund of natural observations … William established anatomy school .. John joined in … and under William’s guidance, john became a professional anatomist and teacher …
John Hunter is well known for popliteal aneurysm repair. Potts noticed by that time that no matter how judiciously performed, proximal and distal ligation of aneurysm would not save the patient’s life. However, John realised that ligating very distally might be able to preserve the collaterals; hence his famous operation, published in London Medical Journal 1786. he decided to approach medially (not posteriorly). He did at St George’s Hospital.
Hunter’s pupils were numerous, including Astley Cooper.
However, his curiosity lead him to inoculate his own penis with a specimen taken from a patient suffering from urethritis. Years later, he developed syphilis and a syphilitic ascending aortic aneurysm.
He then was informed about the appointment of a predecessor in St George’s hospital; he suffered a major angina which proved fatal.
first vein graft –
Alfred Exner from Austria (used canine external jugular vein) then Alexis Carrel from France (University of Lyon). They published their revolutionary idea of using vein as a bypass in 1906 (Surgery, Gyn, and Obst).
Carrel designed the technique, that is still in use now:
A rigid asepsis is absolutely essential for success. . . . The dissection of the vessel is not dangerous if the wall of the vessel is not crushed or roughly handled with metallic forceps of other hard instruments . . . it is necessary that these clamps [vascular] be smooth-jawed and not too strong in the spring . . . by using very sharp, rough needles, only extremely small wounds are made . . . great care is taken not to include fragments of the connective tissue layer in the line of suturing, and to obtain a smooth union and approximation of the endothelial coats.
First clinical anastomosis, however, is sone/published by Jose Guyanese from Madrid. He used an adjacent popliteal vein piece to repair a popliteal aneurysm.
to be continued …
Scottish brothers … born in 1718 and 1728; William was a dedicated educated person .. John never enjoyed books but was fund of natural observations … William established anatomy school .. John joined in … and under William’s guidance, john became a professional anatomist and teacher …
John Hunter is well known for popliteal aneurysm repair. Potts noticed by that time that no matter how judiciously performed, proximal and distal ligation of aneurysm would not save the patient’s life. However, John realised that ligating very distally might be able to preserve the collaterals; hence his famous operation, published in London Medical Journal 1786. he decided to approach medially (not posteriorly). He did at St George’s Hospital.
Hunter’s pupils were numerous, including Astley Cooper.
However, his curiosity lead him to inoculate his own penis with a specimen taken from a patient suffering from urethritis. Years later, he developed syphilis and a syphilitic ascending aortic aneurysm.
He then was informed about the appointment of a predecessor in St George’s hospital; he suffered a major angina which proved fatal.
first vein graft –
Alfred Exner from Austria (used canine external jugular vein) then Alexis Carrel from France (University of Lyon). They published their revolutionary idea of using vein as a bypass in 1906 (Surgery, Gyn, and Obst).
Carrel designed the technique, that is still in use now:
A rigid asepsis is absolutely essential for success. . . . The dissection of the vessel is not dangerous if the wall of the vessel is not crushed or roughly handled with metallic forceps of other hard instruments . . . it is necessary that these clamps [vascular] be smooth-jawed and not too strong in the spring . . . by using very sharp, rough needles, only extremely small wounds are made . . . great care is taken not to include fragments of the connective tissue layer in the line of suturing, and to obtain a smooth union and approximation of the endothelial coats.
First clinical anastomosis, however, is sone/published by Jose Guyanese from Madrid. He used an adjacent popliteal vein piece to repair a popliteal aneurysm.
to be continued …
Bone marrow cell therapy (BMCT) – compared to distal ‘high risk’ bypass
ref. JVS 2015
Bone marrow aspirate injection for treatment of critical limb ischemia with comparison to patients undergoing high-risk bypass grafts
Kristina A. Giles, MD, Eva M. Rzucidlo, MD, Philip P. Goodney, MD, MS, Daniel B. Walsh, MD, Richard J. Powell, MD
outcome are really good ones, and certainly deserve trying in very high risk patients (like the guy I know about) ..
Shunting of carotid artery during CEA: is it useful or harmful
Ref: JVS Jan 2015
The impact of intraoperative shunting on early neurologic outcomes after carotid endarterectomy
Kyla M. Bennett, MD, John E. Scarborough, MD, Mitchell W. Cox, MD, Cynthia K. Shortell, MD
Interesting to see the results:
There was no significant difference in the incidence of postoperative stroke/TIA between the two groups of this matched cohort (3.4% in the no-shunt group vs 3.7% in the shunt group; P = .64).
Analysis of a similarly well matched subgroup of patients with severe stenosis or occlusion of the contralateral carotid artery demonstrated a statistically nonsignificant increase in the incidence of postoperative stroke/TIA with the use of intraoperative shunting (4.9% in the no-shunt group vs 9.8% in the shunt group; P = .08).
My experience in no shunting has been good enough (no postoperative stroke so far)… however, the anaesthetist struggled [seriously] to control the BP where a contralateral stenosis existed .. making me ‘think’ that using a shunt makes life better for the anaesthetist (and patient) in the BP control, no more, no less …
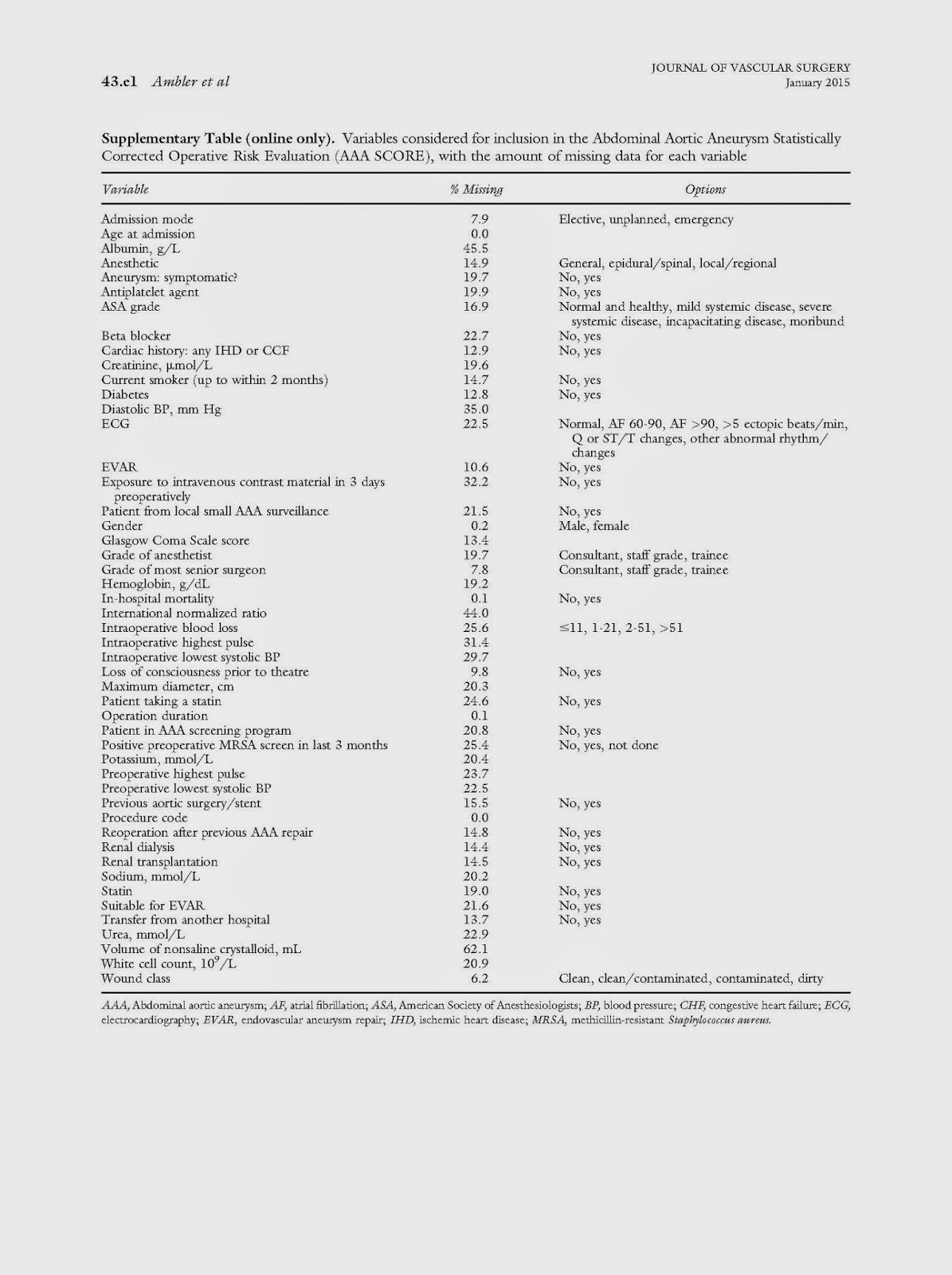
AAA SCORE
Ref. JVS Jan 2015
The Abdominal Aortic Aneurysm Statistically Corrected Operative Risk Evaluation (AAA SCORE) for predicting mortality after open and endovascular interventions
This is a good work aiming at predicting outcome following AAA surgery. The number of parameters used is large (49) but probably should anyway be available in any good quality vascular database.
The Score:
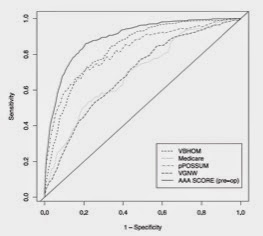
the calibration of this against other predictive models is shown in ROC curve:
This is quite good scoring system.. the main issue lies in the ability to apply it to practice; plus the cases were missing values exist … and of course how much this is going to add to the decision making …
It is also not unreasonable to say that the more factors you use, the better prediction you get … but practical life does not allow that … also, there are certain factors (duration of operation, wound class, etc.) that cn only obtained AFTER operating, not before … all make a scoring system like this not usable in decision making, but rather in (maybe) validating the performance of a unit/surgeon against others, after adjusting to risk (using the score). This is an important part of any quality assurance program in fact, and have certainly a role in current AAA practice.