discussion source:
using the Swedish registry, some 775 patients were identified who underwent intervention for claudication (IC). Those are their results:
Improvement at 1 year was seen in 567 (73.2%) patients, (225 [77.6%] in the open surgery group, 320 [71.6%] in the endovascular treatment group, and 22 [57.9%] in the hybrid treatment group).
No significant difference was found between the open surgery and endovascular treatment groups comprising 737/775 patients (p = .350).
Hybrid treatment gave significantly worse results (p = .046).
Fifty-seven (7.3%) patients reported unchanged limb function and 32 (4.1%) patients reported deterioration.
Within 30 days two patients died and one patient underwent amputation.
Within 1 year 10 patients underwent 11 amputations: five (1.7%) in the open surgery group, three (0.6%) in the endovascular treatment group, and two (7.5%) in the hybrid treatment group; one underwent bilateral amputation (p = .07).
Twenty-two patients died: 10 (3.4%) in the open surgery group, 12 (2.7%) in the endovascular treatment group and none in the hybrid treatment group (p = .465).
My comments:
I do quote my patients a 2% risk of complication following endovascular intervention for IC, and 1% serious complication (amputaion, death, stroke, etc.). This is based on my audit of the Unit results (unofficial). This article from Sweden does reflect almost similiar results; but with death rate of 2-4% which is high.
Would I consider/recommend intervention for IC: well, I do present those figures, discuss in MDT, excludes other pathologies, and give the patient time to think of their quality of life. If all fits, then yes I do offer intervention (this is standard practice in our unit), and usually the patient reaches the rest pain level before I do anything; therefore the risk of them losing their leg is 46% in 6 months (according to TASC II).
when no leg veins are available, should you use the arm veins, or a PTFE?
Arm Vein as an Alternative Autogenous Conduit for Infragenicular Bypass in the Treatment of Critical Limb Ischaemia: A 15 Year Experience. EJVES June 2014
what do we know?
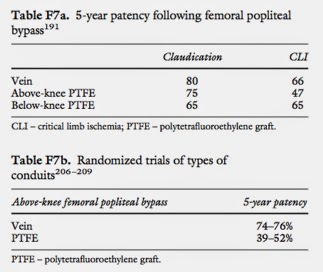
The results for bypass surgery using leg vein vs PTFE are listed in the TASC II guidelines:
What this article tells us:
The authors claim that: The favourable long term results of secondary patency and limb salvage rates encourage the use of arm veins as alternative conduits for infragenicular bypass surgery.
the results are as follows:
The current research shows the following results:
and this is the abstract:
Methods
This was a retrospective study. Between 1991 and 2005. 120 infragenicular bypasses using arm vein conduits (AVCs) were performed in 120 patients. CLI was the main indication (87.5%) for the procedures. The indications for using arm veins were inadequacy or absence of the ipsilateral greater saphenous vein (GSV). Survival, limb salvage, and patency rates were calculated using the Kaplan–Meier method.
Results
There was a predominance of male gender (65%), and the group mean age was 68.1 ± 8.3 years. The mean follow-up period was 29.6 ± 26.3 months. The operative mortality (30 days) rate was 7.5%. The main alternative conduit was non-spliced cephalic vein (37.5%). Composite grafts included GSV + AVC (45.2%), AVC + AVC (43.3%) and small saphenous vein + AVC (11.5%). The 5-year primary and secondary patency (SP) rates were 45.2 ± 5.6% and 56.5 ± 5.0%, respectively. The 5-year SP rate was greatest when using non-spliced cephalic vein (65.8 ± 7.6%), but there was no difference in cumulative patency between spliced and non-spliced veins (49.5 ± 8.0% vs. 61.2 ± 6.4%; p = 0.501). The 5-year limb salvage and survival rates were 70.6 ± 5.9% and 59.6 ± 5.8%, respectively.
my comments:
There is some 10-15% improvement in 5 year patency rate. Out of 10 patients, 4-5 will keep the PTFE graft in 5 years, vs 5-6 in arm veins. If arm vein harvesting is going to be a long operation, then a PTFE with a cuff is probably more suitable. If, however, there is enough staff, and there is a higher risk of infection, then arm veins are likely to be a better alternative.
Is EVAR really better than Open repair in ruptured aneurysms?
Reflections on:
Comments:
Two very interesting points should always be remembered:
- Despite the fact that many observational reports showing significant reduction in 30-day- mortality rate, this systematic review has shown that the improvement does not exceed 10%. It is possible that the trials that managed eventually to recruit patients in such unstable condition has, be default, underwent selection bias toward people with better outcome anyway.
- The physiologic medical logic support the idea that approaching the bleeding (ruptured AAA)via mini invasive surgery would be less harmful and less shocking to doing that with a wider laparotomy incision. The long-term results, however, is not only dependent on the access but also on the overall organ dysfunction during the period from rupture to bleeding cessation. See the comments by Lindholt er al.
Femoral Artery Aneurysms
Femoral artery aneurysms – tips and tricks
Be thorough is assessing: proximal, distal, expected aetiology, possible infection, etc.
Access usually possible via same inguinal incision. Retroperitoneal control is rarely needed.