Protection from, and management of, thrombosis during #coronavirus crisis time: practical advices and evidence-based practice.
CORONAVIRUS AND THROMBOSIS:
With the overwhelming number of Covid-19 patients treated at home, in normal hospital wards, and in intensive care units (ITUs), it has become clear that the number of patients developing clots in lungs, neck arteries, deep venous system, and other body areas is certainly higher than expected. It is now clearly and widely accepted that D-dimer levels, which relates to the thrombosis cascade, is one of the key markers for the severity of Covid-19 cases and the high possibility for developing respiratory failure (ARDS). In a study of 184 ICU patients with proven COVID-19 pneumonia, all of whom received at least standard doses thromboprophylaxis, the cumulative incidence of VTE was 27% and arterial thrombotic of 3.7%. It was noticed that the 31% incidence of thrombotic complications in ICU patients with COVID-19 infections is remarkably high. (Klok et al. Thromb Res 2020 Apr 10. PMID: 32291094). As noticed by the Italian Society on thrombosis, there is a close connection between thrombosis and inflammation, two processes that mutually reinforce each other. There is a spreading feeling therefore that Covid-19 is not uncommonly associated with higher incidence and typical symptoms of disseminated intravascular coagulation (DIC). PMID: 32281926.
Although there is no confirmed evidence as yet, it is quite likely that the plasma of severely-ill Covid-19 patients is hyper-coagulable, as suggested by preliminary laboratory information and many clinical observations. It is also possible that a pulmonary embolism is already present in more severely ill COVID-19 patients BEFORE hospitalisation, thus explaining the reported ineffectiveness of prophylactic doses of heparins during their hospital stay. PMID: 32281926.
OUR RECOMMENDATIONS:
Based on the above, we recommend the following points for all patients with symptoms of Covid-19:
-
FOCUS ON BREATHING EXERCISES:
- Efficiency in acquiring and utilising oxygen has been shown to improve significantly by utilising various structured respiratory patterns (such as using deep breathing techniques) which are able to optimise the delivery of oxygen first to the lungs and then all around the body. (PLoS One. 2012; 7(11): e49074.)
- NICE Guidelines provides some excellent advices on how to improve your breathing capabilities right from the beginning of having any symptoms. This is what to do:
- Use pursed-lip breathing. In here, you should inhale through your nose for several seconds with your mouth closed, then exhale slowly through pursed lips for 4 to 6 seconds. (NICE NG163)
- Correct positioning. Sitting upright can increases your peak ventilation and reduces airway obstruction. (NICE NG163) Try to avoid lying on your back for too long.
- Leaning forward with arms bracing a chair or knees and the upper body supported. (NICE NG163)
- Relaxing and dropping the shoulders. This can reduce the ‘hunched’ posture that comes with anxiety. (NICE NG163)
- NICE also recommend using a trial of Oxygen therapy for patients feeling breathlessness. We recommend to use a regular steamer with breathing exercise to ensure enough oxygenation, humid air, and to soften the mucus plugs that forms during upper respiratory tract infection. Here is one example.
-
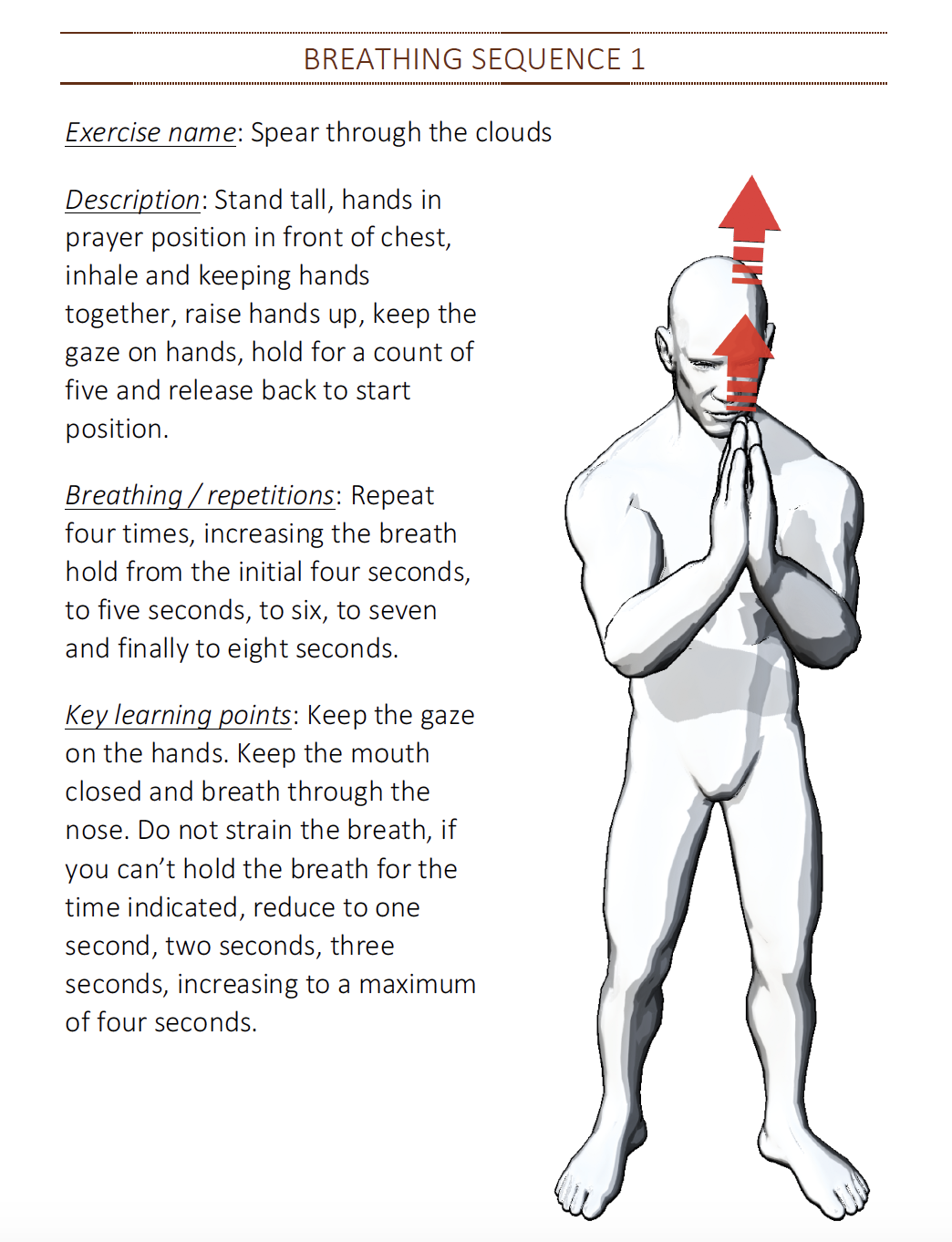
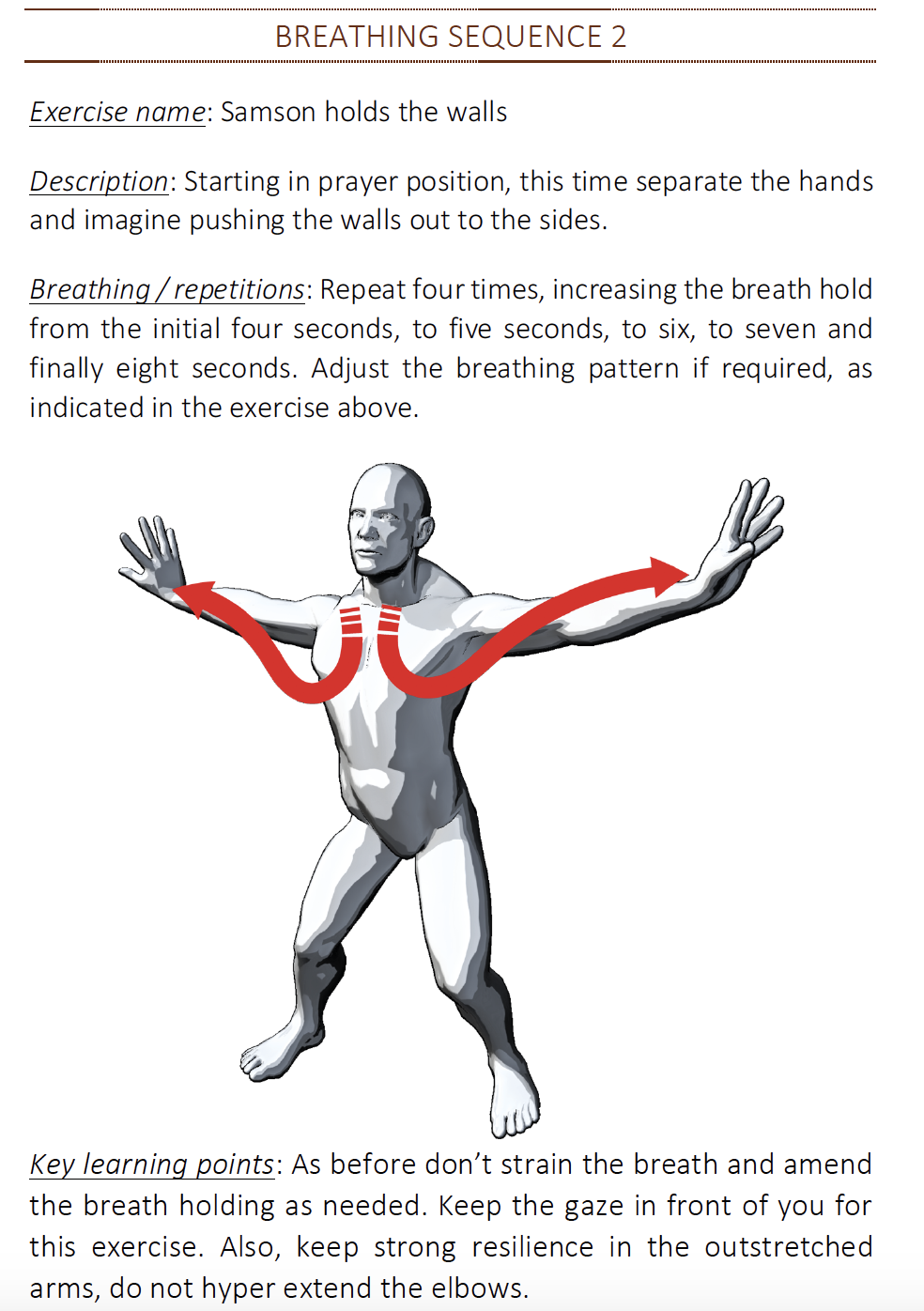
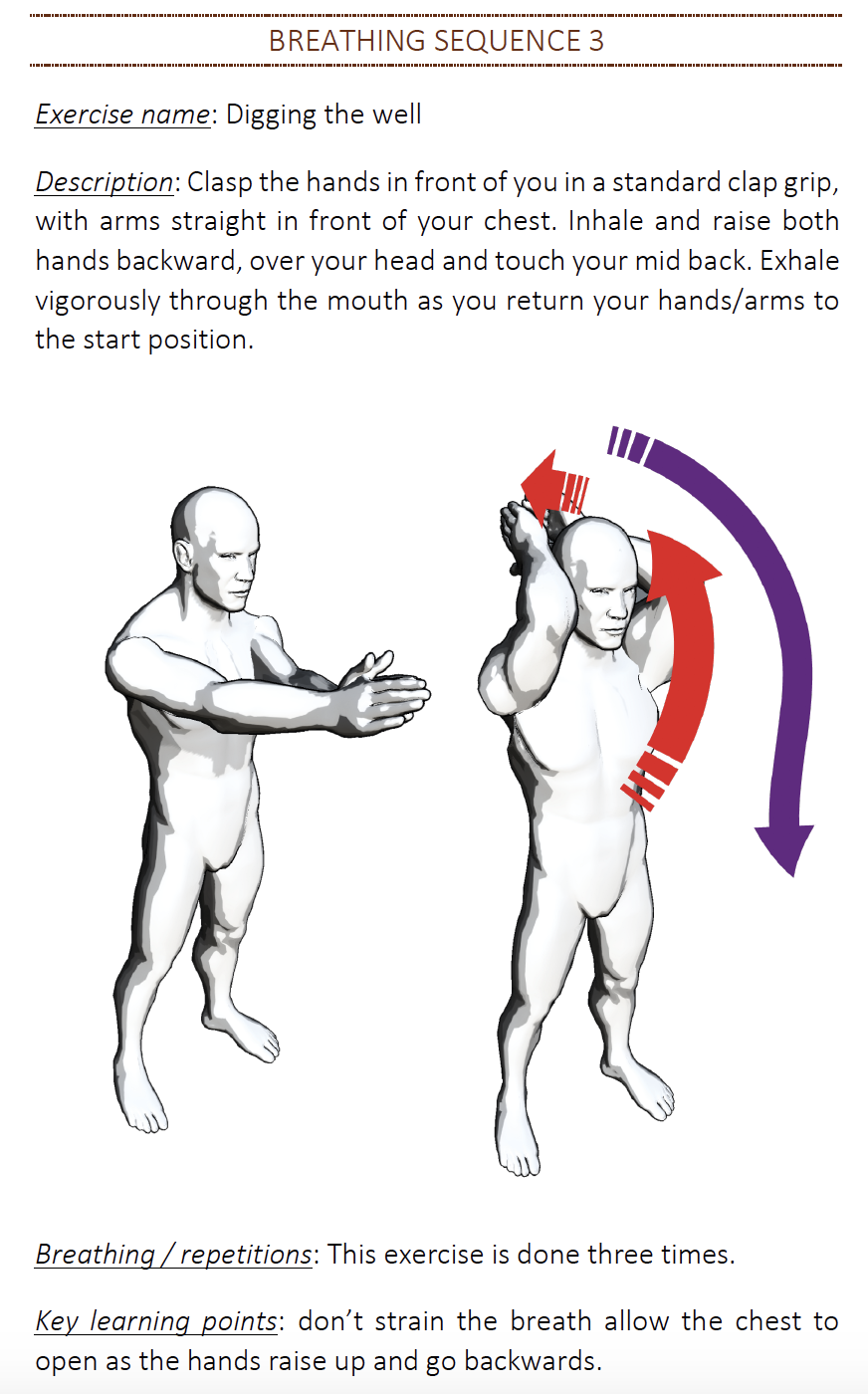
- The following three breathing exercises (taken from my book: Martial Art for Medical Professionals) are selected to maximise your breathing capacity in a structured way:
-
KEEP WELL HYDRATED:
- The second most essential thing to do is to keep well hydrated. NICE guidelines (NICE NG163) recommends keeping the room cool and opening the windows and doors where possible. Hydration has been shown to reduce the risk of DVT (Ref), and ensuring appropriate level of hydration is therefore essential in diseases that are causing higher incidents of DVT (such as Covid-19).
- To keep hydrated, we recommend using an easy to use bottle of water that can be used with minimum efforts and that will ensure you monitor the volume of fluid taken per day. It is quite noticeable that with being tired and weak, dehydration can easily occur. This can often result in deranged kidney function and the development of DVT. One possibility to help in maintaining hydration is to use this type of bottles and to monitor the volume regularly. It has been shown in few patients we managed to be a game changer in maintaining a well hydrated body and provide excellent protection.

-
KEEP TAKING YOUR BLOOD THINNING MEDS:
- If you have been taking Aspirin, Clopidogrel, warfarin, or similar drugs, DO NOT STOP THEM unless advised specifically by your doctor for valid reasons. Due to the high incidence of thrombosis with Covid-19, it is only appropriate to make sure you keep protected by your usual medications.
- If you are NOT taking any blood thinning medications before, there is currently NO RECOMMENDATIONS to start them. It might be possible in the future for this advice to change, especially in patients of high risk of thrombosis such as heavy smokers or patients with previous DVT. Currently, we only recommend keeping active and keeping well hydrated.
- If you are admitted to hospital for severe COVID-19, it is very likely that your physicians will ensure you are well protected with a prophylactic blood thinning tablets or injections. Most guidelines for the management of Covid-19 are focusing on this important part of treatment.
-
KEEP REGULAR EXERCISES:
- Thrombosis and DVTs are more common in patients with sedentary life style. In addition, regular exercises have been shown to boost the immune system significantly, and therefore help in fighting against viral infection such as Covid-19.
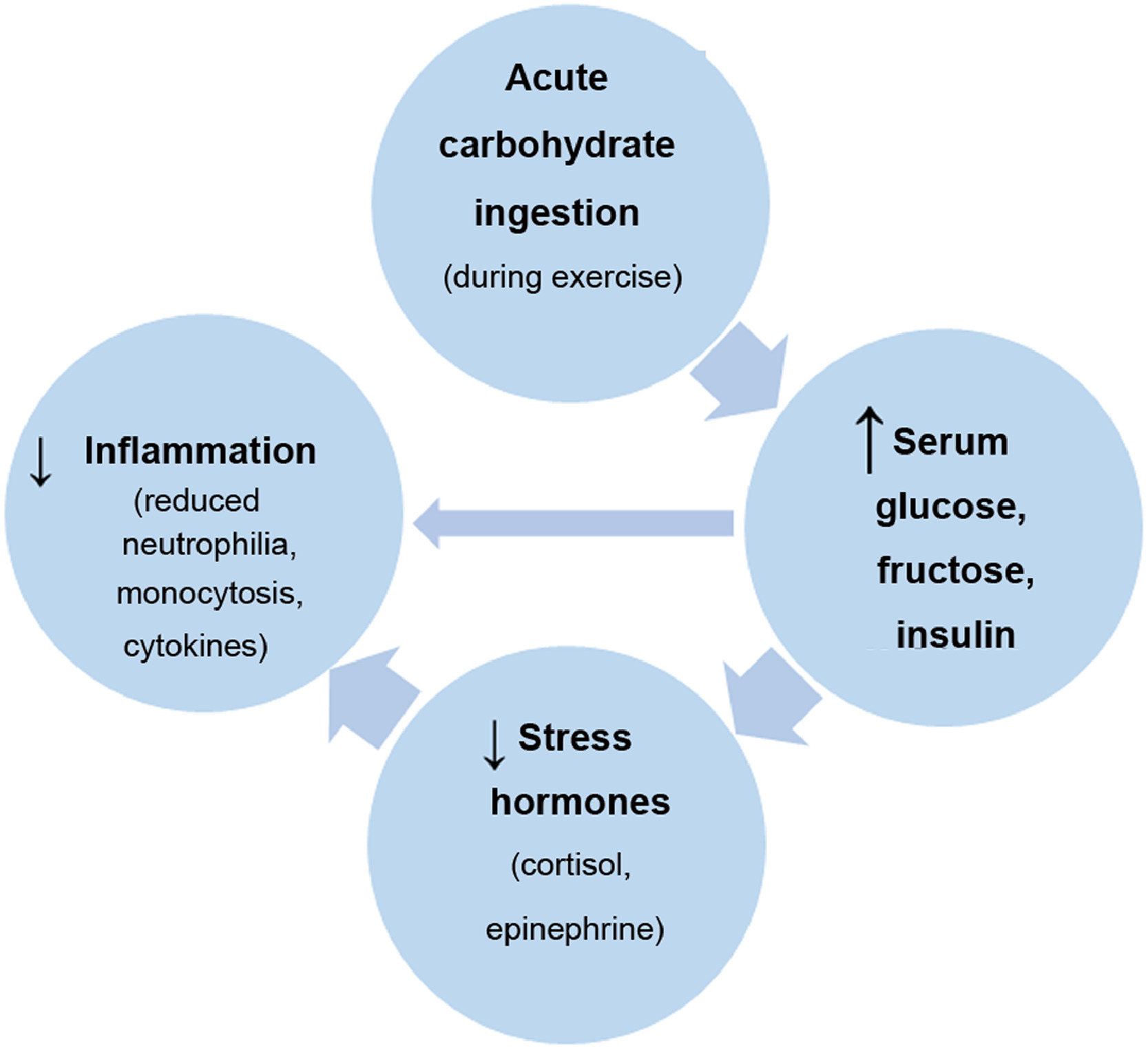
- A recent review article (J Sport Health Sci. 2019 May; 8(3): 201–217) has shown that acute exercise is an immune system adjuvant that improves defence activity and metabolic health. Data supports a clear inverse relationship between moderate exercise training and illness risk. In fact, exercise training has an anti-inflammatory influence mediated through multiple pathways.
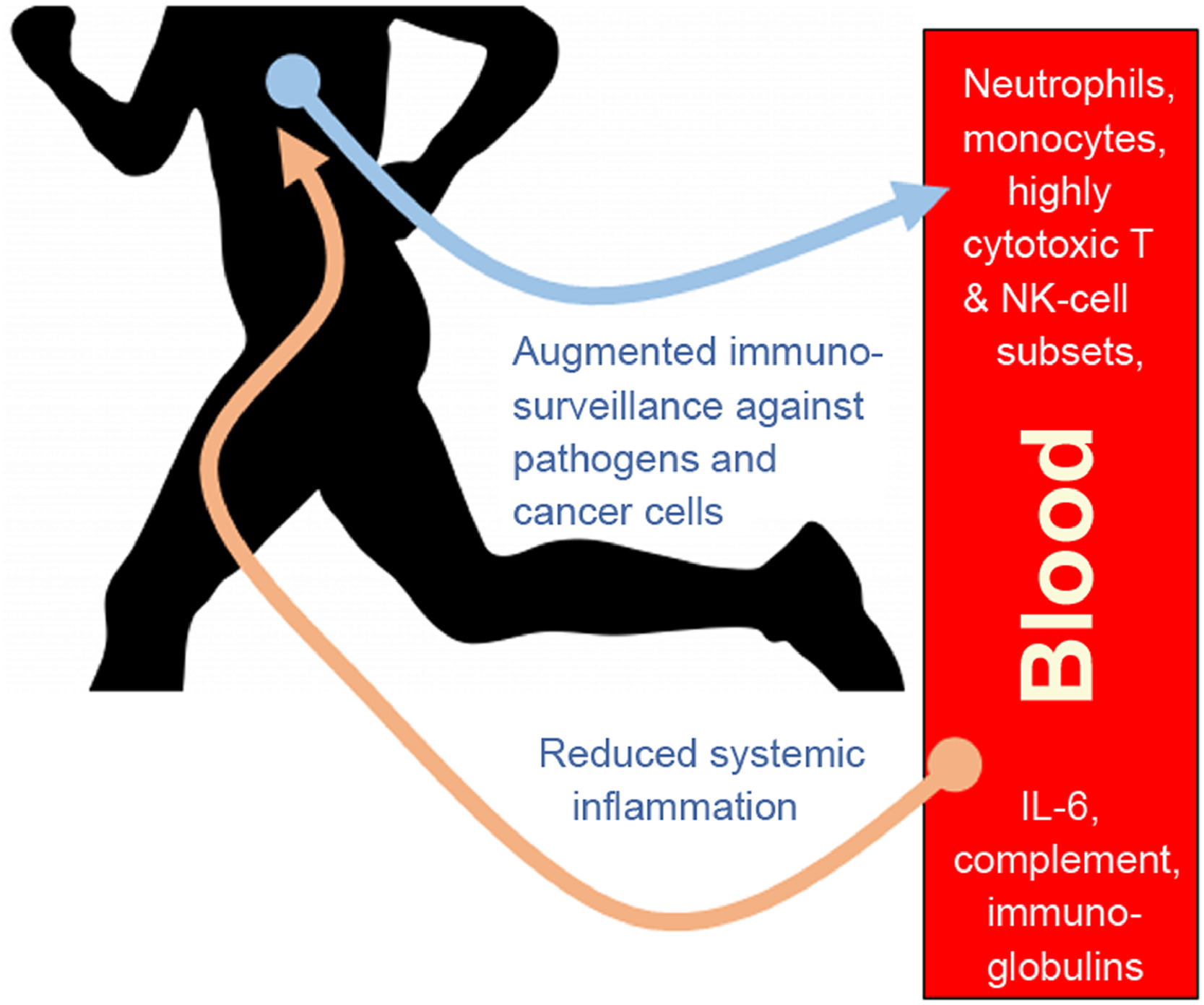
- We do therefore highly recommend having a regular exercise programme on a daily basis, especially for patients with symptoms (or confirmed) Covid-19. This minor regular activity will make all the difference to your wellbeing, your resilience, your protection from DVT, and your ability to fight.
-
GET ENOUGH SLEEP:
-
- Poor sleeping, including obstruction sleep apnea, has been shown in systematic reviews to increase the risk of developing DVT. (Thromb Haemost 2015 Nov;114(5):958-63). In addition, sleep disruption has been shown to badly affect the immune system and increase the risk of infection (Brief Definitive Report February 12 2019). Getting enough sleep and monitoring that is therefore essential for protection from DVT and enhancing the immune system.
- We do recommend using a smart watch with the ability to monitor your sleeping to ensure you are having good and enough sleep every night and to compensate for that if this is affected.


-
-
EAT WELL:
- Finally, you need to focus on your eating habits. Although there is no “strong scientific evidence” for any specific type of food being linked to better immune function, there are certain type of diet and supplements that should not be deficient in your body during this period:
-
- Vitamin D – Around one-quarter of the UK population is deficient in vitamin D, rising to around one-third in the winter months. It is now clear that vitamin D has important roles in addition to its classic effects on calcium and bone homeostasis. Deficiency in vitamin D is associated with increased autoimmunity as well as an increased susceptibility to infection. (J Investig Med. 2011 Aug; 59(6): 881–886).
- We recommend taking a regular Vit D supplement during the winter time at least. Make this a regular habit on a daily basis especially of your have symptoms of Covid-19.
- Zinc – Zinc is an essential trace element for humans. Zinc is required for the function of over 300 enzymes and 1000 transcription factors. Cardiovascular health is strongly influenced by diet. Zinc has antioxidant and anti-inflammatory properties. Studies have demonstrated that suboptimal dietary zinc intake raises circulating pro-atherogenic lipoprotein levels that promote vascular inflammation and enhance arterial plaque formation.Zinc has also be shown to exhibit direct and indirect antimicrobial effect when it is release from immune cells (all granulocytes secrete zinc). Zinc supplementation is recommended where there is high risk of zinc deficiency as a preventive measure. A Cochrane review suggested that people taking zinc supplement may be less likely to progress to age-related macular degeneration.
- Vitamin D – Around one-quarter of the UK population is deficient in vitamin D, rising to around one-third in the winter months. It is now clear that vitamin D has important roles in addition to its classic effects on calcium and bone homeostasis. Deficiency in vitamin D is associated with increased autoimmunity as well as an increased susceptibility to infection. (J Investig Med. 2011 Aug; 59(6): 881–886).
-
- Other Dietary supplements that can be useful (despite lack of high level evidence for most):
-
- Ginger (Zingiber officinale), has become increasingly popular for its antiemetic and osteoarthritis-alleviation properties [2]. An open label, three‐way crossover randomized study conducted on healthy subjects by Jiang et al. in 2005 found that Blackmores Travel Calm Ginger (equivalent to 0.4 g of ginger rhizome powder) did not significantly impact blood’s ability to clot [7] The Food and Drug Administration (FDA) however advised healthcare providers to be cautious in patients who are on warfarin and who also use ginger, garlic, and other dietary and herbal supplements [3].
- Vitamin E rich foods like walnuts, spinach, sunflower seeds, olive oil, bell peppers and kiwis benefit people experiencing oxidative stress due to free radicals when administered at the correct time and for an appropriate duration.(Korean J Intern Med. 2015 Sep; 30(5): 571–579). Data from data the Women’s health study suggest that supplementation with vitamin E may reduce the risk of VTE in women, and those with a prior history or genetic predisposition may particularly benefit. (Circulation. 2007 Sep 25;116(13):1497-503) For this reason and for many other reasons, we highly recommend using green vegetables in the diet during this period.
- Garlic gloves have been shown in some studies to be able to reduce the adherence of platelets, and therefore reduce the thrombosis risk. (Prostaglandins Leukot Essent Fatty Acids .1995 Sep;53(3):211-2.) The evidence however is not the strongest.
- Cinnamon has a natural anticoagulant called coumarin that helps in lowering blood pressure as well acts as a blood thinner promoting blood circulation and preventing blood clots. (Clin Nutr. 2019 Apr;38(2):594-602.).
- Other home remedies that might be of benefit include using honey (NICE Guidelines NICE NG163) and possible use of Black seed oil (Asian Pac J Trop Biomed. 2013 May; 3(5): 337–352.)
-
- Finally, you need to focus on your eating habits. Although there is no “strong scientific evidence” for any specific type of food being linked to better immune function, there are certain type of diet and supplements that should not be deficient in your body during this period:
- Don’t stress. “Stress hormones such as cortisol can compromise immune function’ says professor Arne Akbar of the British Society for Immunology.
In summary, it is essential to maintain basic well-being activities in order to fight effectively against Covid-19 (and other viral infections). Thrombosis is one aspect of this fight, and maintaining a healthy blood haemostats has therefore become a key step in winning this fight.
Got a question ? We are more than happy to help. We can arrange a remote consultation for you and your family members. Contact us at @AJLYON.co.uk or directly message us. Our average response time is 24h or less.
Stay at home, protect the NHS, Save Lives! #StayHomeSaveLives
Get official and uptodate advice from: gov.uk/coronavirus