the answer is NO; no supporting evidence from major carotid registries in the world according to Prof Naylor’s report.
Ref. EJVES Jan 2016
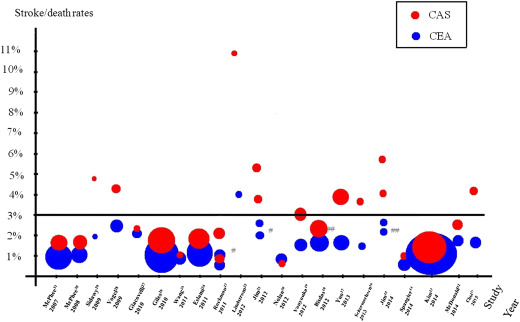
Stroke/death rates for “average risk” asymptomatic patients undergoing CAS and CEA in various registries. #Results reported separately for patients aged <65 and ≥65 years.
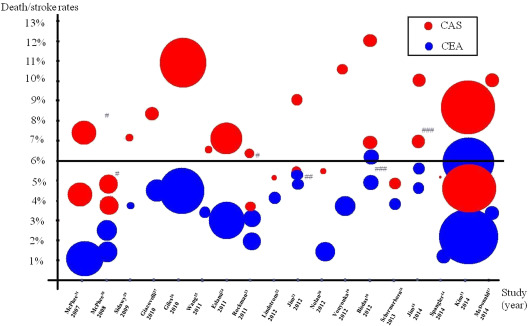
Stroke/death rates for “average risk” symptomatic patients undergoing CAS and CEA in various registries. #Stroke and death rates reported separately. ##Stroke/death rates reported separately for patients aged <65 and ≥65 years.