As far as travelling with airlines in patients with AAA is concerned, the NHS screening programme reports that the Association of British Insurers (ABI) has been advised that AAAs are no more likely to rupture at altitude than on the ground and it is not aware of any airlines operating a standing rule about refusing patients with this condition. The ABI is also unaware of any travel insurance policies that contain a specific exclusion for AAAs as part of their standard wording.
Stopping smoking – a patient’s story
This story is impressive in all aspects .. and Pat has agreed to spread the word for generations to come .. the publisher is Ashford and St Peter’s Hospital NHS Foundation Trust:
http://www.ashfordstpeters.nhs.uk/gp-news/1211-stopping-smoking-a-patient-s-story
Stopping smoking – a patient’s story
Dear Mr Jibawi, I thought I’d drop you this note about my smoking and to say thank you for all your hard work in keeping me alive!
I started smoking when I was 14 years old. In those days a schoolgirl (or boy!) could buy one cigarette, two matches and a bag of crisps for two old pence from the local corner shop. Some 54 years and myriad operations later (I’ve had three operations for cancer and two to try to save my leg in the last 13 months alone) I’ve at last stopped smoking.
Every time over the years, whenever I’ve needed an operation or had a chest infection, I’ve always been told “You have to stop smoking. It’s going to kill you”. And, of course, I always thought “You have to tell me that, maybe it’s required by law or something!” And anyway, I told myself, I didn’t smoke much, and I was still young and had plenty of time. And of course, death is something that happens to other people, by a fatal accident or when you get really, really old.
And then I started with the horrendous claudication pain in my left leg, which led me to you. I knew immediately what it was, having had the same problem ten years previously in my right leg. Having attended your outpatients clinic on 2nd June last year, Dr Anneleise Lawn told me that I simply had to stop smoking. I saw you later that month and in your subsequent letter to my GP (copied to me) you were much more outspoken, telling him that if I didn’t have an operation before Christmas there was a 42% risk that my leg would need to be amputated within six months with the very real associated risk of death. As you can imagine, that really made me sit up and take notice. Whilst I’ve been told verbally many many times, there’s something about having it in black and white in front of you that you can’t escape from.
So, in June last year I stopped smoking tobacco. On the advice of Dr Lawn I bought some e-cigarette batteries and cartridges and can truly say I haven’t missed cigarettes at all. I started on 1.8% nicotine strength cartridges (the equivalent of the low tar cigarettes I was previously smoking) and am now on the 0% nicotine cartridges and will soon stop those as well.
So … thank you for your directness, and for your skill and for putting such a good team together. And five weeks after the second operation and an arterial bypass (I seem to recall a certain surgeon telling me I had “terrible arteries, terrible!”) I’m now walking between three-quarters and one mile every day.
Pat Smith
Music for surgeons ,, for patients ,, or for staff??
well .. the evidence sounds quite conflicting …
The Lancet (Aug 2015) published a systematic review and a meta-analysis of 73 RCTs, showing a significant improvement in patient’s level of anxiety and pain. The evidence is good and the message is clear. Results are linked herein.
Music for surgeons has long ben known to promote a positive mind and to enhance surgery. It has been shown, in the case of plastic surgeons, to improve timing by 10% or more. Music has been shown to improve performance in laparoscopic simulation surgery, and on the cardiovascular reactivity among surgeons.
Nurses, however, were not in quite agreement with this. Music generally caused more distraction and inability to hear surgeon’s instruction than it helped in relaxing the scrub nurses.
The question then remains in who is more important: an euphoric surgeon who can perform better, a more relaxed and less painful surgery to the patient, or a happier scrub nurse? I guess this has to be judged at the very individual setting. I am afraid that in many cases, the nurse becomes the most disadvantaged!
Here is a good article from the Independent: http://www.independent.co.uk/life-style/health-and-families/features/the-best-music-for-surgery-and-who-should-be-allowed-to-choose-it-10462792.html
Direct anticoagulants & preop policy
The half life of RIVAROXABAN is 5-9h in healthy individuals and 11-13h in the elderly. Ref.drugs.con
In uptodate.com: RIV can be stopped 2-3days before a procedure, with shorter interval if procedure has low risk of bleeding, based on or with no renal failure who is receiving 20mg once daily doses, or moderate renal failure on 15mg od.
RIV can only be checked if really needed usingantifactor 10 levels.
In rare cases, bridging is required, such as pts with very high thromboembolic tendency.
RIV can be reinstituted immediately after procedure once haemostats is achieved, at the same dose, providing there is no big risk of further bleeding.
RIV costs £63 for 20mg 30-tab pack.
Warfarin, in comparison, costs £1.07 for 5mg 28-tab pack
Which is better long-term: endovenous laser ablation or traditional surgery for varicose veins?
Ref: EJVES Nov 2015
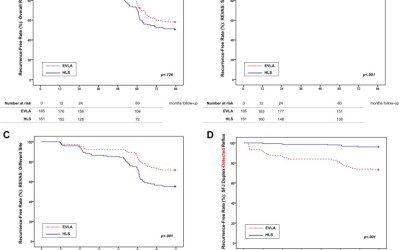
This is seriously interesting!! Most, if not all, surgeons have now ‘switched to’ endovenous thermal ablation (laser or RF). The endovenous therapy has proven safety and mid-term results. what about the long term recurrence? RELACS study has some logic : traditional surgery risks the recurrence to occur in the site of operation; the endothermic risks the recurrence to occur in other places. Here are the results:
Same Site Recurrence is More Frequent After Endovenous Laser Ablation Compared with High Ligation and Stripping of the Great Saphenous Vein: 5 year Results of a Randomized Clinical Trial (RELACS Study)
Interventions were performed on ambulatory and hospitalized patients at two vein centres, a university dermatology department (EVLA) and a specialized vein clinic (HLS). Four hundred patients suffering from GSV incompetence were assigned to EVLA or HLS of the GSV. One hundred and eighty five and 161 patients (=limbs), respectively, were treated per protocol. Main outcome measures were clinically recurrent varicose veins after surgery (REVAS classification, primary study objective), Duplex detected saphenofemoral recurrence, clinical venous severity scoring (Homburg Varicose Vein Severity Score), quality of life (Chronic Venous Insufficiency Questionnaire 2), side effects, and patient satisfaction 5 years after treatment.
Results
- Two hundred and eighty one legs (81% of the study population) were evaluated with a median follow up of 60.4 (EVLA) and 60.7 months (HLS).
- Overall, REVAS was similarly observed in both groups: 45% (EVLA) and 54% (HLS), p = .152.
- Patients of the EVLA group showed significantly more clinical recurrences in the operated region (REVAS: same site): 18% vs. 5%, p = .002.
- In contrast, more different site recurrences were observed in the HLS group: 50% vs. 31%, p = .002.
- Duplex detected saphenofemoral refluxes occurred more frequently after EVLA: 28% vs. 5%, p < .001.
- Both treatments improved disease severity and quality of life without any difference.
The results are summarised in this good figure:
The figure is shown for educational purposes only and not for reuse.
Conclusion – don’t take it for granted!! need more work on best treatment options …
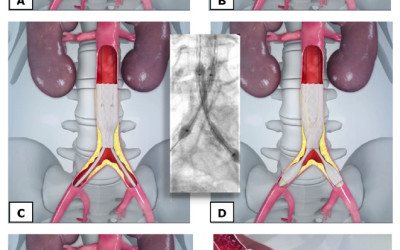
CERAB technique to replace aorto-bifemoral bypass .. is heating up!
Ref: EJVES Nov 2015
This is the editor’s choice for EJVES this month… and it deserves!! It is a new era in major vascular reconstruction, now been followed for 0-48 months with excellent results so far. The study took place in the Netherlands and in Belgium.
The procedure is simply to use covered stents after passing the iliac and aortic blockage with wires and catheters.
picture taken from CERAB original description for educational purposes only. http://www.angiocare.nl/uploads/downloads/4.CERAB_ZNA_poster-(1).pdf
The idea resembles the EVAR technique, with three key differences: passing wires through blockages; landing in a less-than-average aortic diameter, and lack of further attachments (barbs, hooks, etc.).
Between 2009 and March 2014, 103 patients (51 male, 52 female) suffering from obstructive lesions at the level of the aortic bifurcation were treated with CERAB in two clinics. The median age was 61 years (range 36–85 years). Lesion morphology was evaluated by CT angiography. Six TASC-II B lesions, nine TASC-II C lesions, and 88 TASC-II D lesions were treated. Follow up was a median 12 months (range 0–49 months) and consisted of clinical examination, ankle brachial indices, and duplex ultrasound examination.
- Technical success was obtained in 98 procedures (95.1%). In five cases lesions could not be recanalized.
- Primary patency was 87.3% at 1 year and 82.3% at 2 years, while secondary patency was 95.0% at 1 year and 95.0% at 2 years.
- Mean ankle brachial indices improved significantly from 0.64 ± 0.21 before to 0.91 ± 014, after the procedure (p < .001).
- The overall 30 day complication rate was 23.3%, including 22 minor complications and two major complications (1.9%).
- There was no 30 day mortality. Median hospital stay was 2 days (range 1–16 days).
What this paper adds
The study is an evaluation of the first (and largest) patient cohort, showing the safety and excellent patency of this technique when treating aortoiliac arterial occlusive disease. There seem to be a potential shift from open surgical bypass grafting to endovascular treatment for patients suffering from disabling intermittent claudication or critical limb schema. We need more info and longer term results to judge; but the astonishing 0% mortality and 2 day LOS is impressive so far, not to mention the 95% technical success rate.
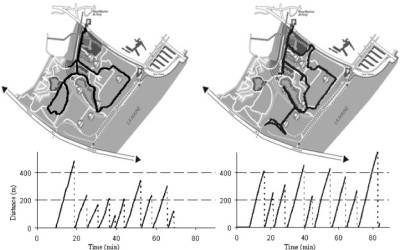
How efficient it is to use GPS in monitoring intermittent claudicants?
ref: EJVES Nov 2015
Reports are emerging on using modern ‘wearable’ technologies in monitoring outcome for cluadicants. The number of patients is still low, but the idea and the statistical design and analysis are the interesting part.
In this French study, seventeen PAD patients performed two series of evaluations (T1 and T2) within a 1 month period. Each series included: a 1 hour stroll in the community with the calculation of the walking impairment questionnaire (WIQ) scores, the measurement of maximal walking distance on a treadmill (MWD on treadmill) and a 1 hour stroll in the community with GPS. Test-retest reliability of MWD on treadmill, WIQ, and GPS parameters were assessed with intraclass coefficient of correlation (ICC).
ICCs are almost perfect between T1 and T2 for greatest distance (ICC = 0.911), average speed (ICC = 0.905), and MWD on treadmill (ICC = 0.992), and substantial for the average WIQ (ICC = 0.794). Correlation of average stop durations was considered substantial (ICC = 0.691).
This figure provides an example of the recordings observed during the two strolls (Test 1 and Test 2) in the same patient. The figure is a copyrighted material and is not reusable. It has been used here for the sole purpose of education.
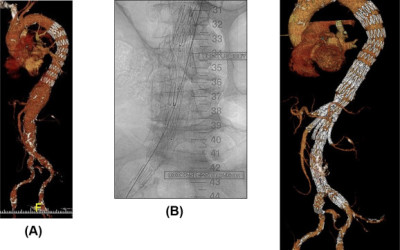
Spinal cord ischaemia in thoracic aneurysm endovascular repairs – major centres are now saying it is ‘preventable’!
Ref. EJVES Nov 2015
The work and results coming from ST Thomas’ Unit in London are, to say the least, very encouraging. SCIs are not only preventable, but they are SIGNIFICANTLY reversible! This is quite encouraging when advising patients. We of course has to remember one important point: attention to details by the WHOLE team, not only by the surgeon!
Here are some details:
- Sixty-nine patients (median age 73 years, 52 male; Crawford classification type I [n = 4], type II [n = 11], type III [n = 33], type IV [n = 14], type V [n = 7]) underwent endovascular TAAA repair.
- Twelve patients developed neurological symptoms/signs related to SCI
- This was successfully reversed in eight patients, leaving four (5.8%) with permanent paraplegia.
- The median length of aorta covered was not significantly different in the 12 patients who developed SCI compared with the cohort that did not. see picture!
- Eleven of the patients who developed SCI had an intraoperative mean arterial pressure (MAP) below 80 mmHg. Cutaneous atheroemboli were noted in half of the patients in the SCI group compared with 11% of the non-SCI group (p < .05).
- Strategies used to reverse SCI included raising MAP, cerebrospinal fluid drainage, angioplasty of stenosed internal iliac arteries, and restoring perfusion to the aneurysm sac.
Picture: notice the extent of aortic coverage. This did not affect the incidence of SCI. Picture for education purpose and news reporting only and is not reusable.
When should we consider carotid lesion as ‘highly vulnerable’ regardless of symptoms?
Ref: EJVES Nov 2015
This question has no clear unquestionable answer unfortunately! If you pick up a ‘highly vulnerable’ lesion in asymptomatic patient, who has no stroke history and referred, electively, to your clinic, then you still have to think TWICE! Adding haemodynamic data to static ones may also help you in the decision: finding small ‘blebs’ on doppler scan for example, or from a more accurate dynamic imaging in the future, would certainly help convincing both you and the patient that there is a dangerous plaque here. If you adopt a policy in the centre to operate on asymptomatic patients with significant stenosis (or with highly vulnerable plaque), then your results should follow the major trial results, and you would be able to estimate how many have you helped before one was harmed!
In this work from Toby Richards and team at UCL, highly vulnerable lesions were considered as those having several structural plaque characteristics that distinguish the “vulnerable” from the “non-vulnerable” plaque, which includes plaque ulceration, intraplaque haemorrhage (IPH), thin or ruptured fibrous cap (FC), lipid-rich necrotic core, and the presence of calcification. (1) Inflammation may also play a role in the development and progression of disease as well as identifying the vulnerable plaque.(2)
(1) A.V. Finn, M. Nakano, J. Narula, F.D. Kolodgie, R. Vierman. Concept of vulnerable/unstable plaque. Arterioscler Thromb Vasc Biol, 30 (2010), pp. 1282–1292
(2)M. Marnane, S. Prendeville, C. McDonnell, I. Noone, M. Barry, M. Crowe, et al. Plaque inflammation and unstable morphology are associated with early stroke recurrence in symptomatic carotid stenosis. Stroke, 45 (2014), pp. 801–806
The conclusion is even more interesting:
US, CT, MRI, and PET are non-invasive imaging techniques that show promise for identifying vulnerable plaque characteristics beyond the degree of stenosis.
Although the aforementioned imaging parameters are promising, at present there is no single imaging technique that can clearly identify the vulnerable plaque. This is because (a) there is no single imaging modality that can detect all vulnerable plaque features, (b) plaque imaging is expensive, time-consuming, and requires a reviewer with advanced experience, and (c) prospective natural follow-up studies analysing the value of these imaging modalities for future cerebral events are limited. It is therefore important to realise that even if we could reliable identify ulceration, LRC, thin FC, and IPH as characteristics of the vulnerable plaque, at this stage there is not enough evidence that these patients indeed have a higher risk of stroke.
MRI has the most potential, with good sensitivity and specificity for most plaque characteristics, of course, within the above limitations …